A 60year old male agricultural worker by occupation resident of gudivada (Nalgonda)came to hospital with complaints of swelling on upper and lower limbs ,face since 1 week

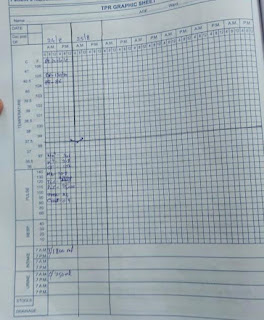
October 17, 2023 Hi I am, Madhuri palsa 5 th sem medical student. This is an online e-log book to discuss our patient's health data shared after taking his/her consent . This also reflects my patient centered care and online learning portfolio. A 60year old male agricultural worker by occupation resident of gudivada (Nalgonda)came to hospital with complaints of swelling on upper and lower limbs ,face since 1 week Chief complaints Patient complaints of swelling in limbs and face since 1 week History of presenting illness Patient was apparently asymptomatic 1 week back He then developed swelling of body -upper limbs,lower limbs and face Pitting type, insidious onset and gradually progressive Complaint of chest pain,palpitation and decreased urine output SOB Ulcer over sacral region History of past illness Not a known case of Diabetes Hypertension Epilepsy Asthma Tuberculosis No history of trauma in the past Personal history Sleep:adequate Diet: mixed Bowel and bladder moveme